A cellular system makes the battle against a rare disease personal
Mitochondria, compartments in cells that produce most of its energy, are unique in that they carry their own DNA, which is inherited only from a person's mother. Mutations in mitochondrial genes often cause neurological conditions because nerve cells need high levels of energy for their function.
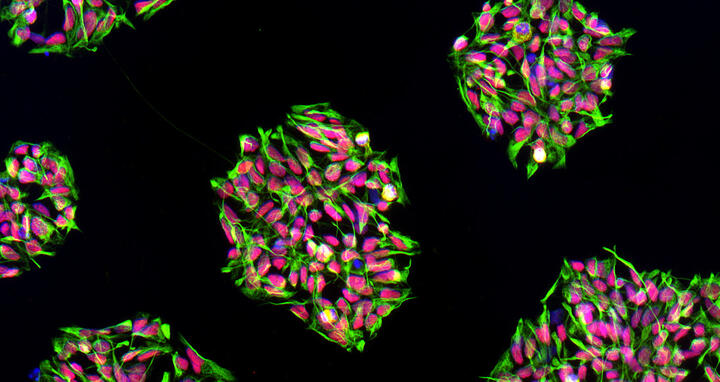
These are colonies of neural progenitor cells, which were derived from human induced pluripotent stem cells. Colors code for proteins specific for the cell type. Image: Gizem Inak, Prigione Team, MDC
Recently it has become possible to solve this problem for mothers bearing a mitochondrial mutation. Scientists can replace the mitochondria of the mother's egg cell with mitochondria from a healthy donor. This gives the baby three genetic parents: DNA in the nucleus from the mother and father, and that of the mitochondria from the donor.
This strategy is not an option for every family that carries a mitochondrial mutation. Most countries do not allow scientists to modify human egg cells. And the strategy is purely preventative – it will not help children who have already inherited mutations. This has motivated groups such as that of Alessandro Prigione at the MDC to continue to search for other solutions.
Why research of mitochondrial diseases is hard
“A major reason we lack good models to investigate such diseases is that the highly refined techniques we use to modify genes in the nucleus don't work for mitochondrial DNA,” Prigione says. “This causes a lack of animal models. Cell culture systems used today also do not faithfully represent the features of human neurons”. A major challenge has been to find a way to better understand the way the disease affects human nerve cells.
Another issue is that it would be important to observe the effects of drugs on cells – specifically the types that are hardest hit by the disease – before administering them to patients. A skin cell, which is fairly easy to raise in the lab, copes very differently with faulty mitochondria than a nerve cell. A drug might affect them in completely different ways.
A new strategy for drug screens
Prigione and his team may now have solved these problems in one fell swoop and published their findings in Cell Stem Cell. With PhD student Carmen Lorenz at the MDC and the Berlin Institute of Health (BIH), he teamed up with other MDC researchers and scientists from France to come up with a new cell-based system to carry out drug screens.
The strategy involves extracting skin cells from patients with faulty mitochondria and reverting them to a more basic type of cell called an induced pluripotent stem cell (iPS cell). These can now be “reprogrammed” to assume another fate, such as the neurons affected by mitochondrial disease.
“It was crucial to establish a cellular system with similar characteristics of the affected nerve cells in the patients," Prigione says. "We discovered that neural progenitor cells show properties that can be associated with the disease and were perfectly suitable for use in large-scale drug screens.”A number of tests demonstrated that these artificially created cells had all of the properties of the affected nerves, including the calcium imbalance and reduced energy production observed in patients.
These are neurons differentiating from colonies of neural progenitors, which were derived from human induced pluripotent stem cells. Image: Gizem Inak, Prigione Team, MDC
Promising first experiments
The next step was to expose the neural progenitor cells to 130 substances that had already been approved by the FDA for use in treating other diseases. Functional measurements of the cells showed that a drug called avanafil reversed some of the cellular imbalances caused by the mitochondrial defect.
“Avanafil is an approved drug, which is extremely promising," Prigione says. "We can directly move to the next step of trials in human patients. We're preparing for this at the moment. We're also continuing to test a lot more compounds. Once you have a good model system, you can screen the several thousand drugs already approved by the FDA. This creates the potential of developing truly personalized treatments – even for very rare diseases."
Carmen Lorenz1,2, Pierre Lesimple3,4,5, Raul Bukowiecki1, Annika Zink1,6, Gizem Inak1, Barbara Mlody1, Manvendra Singh1, Marcus Semtner1, Nancy Mah6, Karine Auré3,4,5, Megan Leong1, Oleksandr Zabiegalov1, Ekaterini-Maria Lyras6, Vanessa Pfiffer1, Beatrix Fauler7, Jenny Eichhorst9, Burkhard Wiesner9, Norbert Huebner1, Josef Priller2,6,8, Thorsten Mielke7, David Meierhofer7, Zsuzsanna Izsvák1, Jochen C. Meier1,10, Frédéric Bouillaud3,4,5, James Adjaye11, Markus Schuelke6, Erich E. Wanker1, Anne Lombès3,4,5, Alessandro Prigione1 (2017): “Human iPSC-derived neuronal progenitors are an effective drug discovery model for neurological mitochondrial DNA disorders.” Cell Stem Cell. doi:10.1016/j.stem.2016.12.013
1Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC), Berlin, Germany; 2Berlin Institute of Health (BIH), Berlin, Germany 3INSERM, Institut Cochin, Paris, France; 4CNRS, Paris, France; 5Université Paris Descartes, France; 6Charité Universitätsmedizin, Berlin, Germany; 7Max Planck Institute for Molecular Genetics, Berlin, Germany; 8DZNE, Berlin, Germany; 9Leibniz Institut für Molekulare Pharmakologie (FMP), Berlin, Germany; 10Zoological Institute, Braunschweig, Germany; 11Institute for stem cell research and regenerative medicine, Medical Faculty, Heinrich Heine University, Düsseldorf, Germany
Carmen Lorenz and Pierre Lesimple are first co-authors. Anne Lombès and Alessandro Prigione are senior co-authors.
Contact
Vera Glaßer
Max Delbrück Center for Molecular Medicine (MDC) Berlin-Buch
Head of Communications department (interim)
Tel: +49 30 94 06 - 2120
presse@mdc-berlin.de