Too much salt confuses the immune system
For a long time doctors have warned that a high-salt diet drives blood pressure upwards, increasing a person's risk of suffering a stroke or heart attack. Now scientists have discovered that salt influences the immune system as well. A team of researchers led by Dominik Müller from the Experimental and Clinical Research Center of the MDC in Berlin-Buch and the Charité – Universitätsmedizin Berlin has discovered a new mechanism by which salt upsets the equilibrium of the immune system. Their findings were recently published in the Journal of Clinical Investigation.
In excess it is harmful, but we cannot live entirely without it: table salt (sodium chloride) is vital to our health because it regulates the water balance of our bodies. Most of the excess salt that we ingest with our food is excreted through the kidneys, but not all. A few years ago, in a project with scientists from other institutes, Dominik Müller showed that our body can also store salt – not in the blood, but in a rather unexpected location: the skin.
This salt is deposited in the interstitium – the space between cells – whose functions go beyond this role as a salt reservoir. During an infection, immune cells migrate to the skin, and their activity depends on the environment they find there. Could salt in the interstitium affect their functions? The answer, according to a number of studies, is a definitive "yes". One effect of high levels of salt is to increase the number of Th17 cells, a subgroup of T helper cells; another is to alter the activity of phagocytes called type 1 macrophages.
“This came as a surprise to many immune researchers,“ Müller says. “Since those initial findings, we have been trying to gain a deeper understanding of the significance of salt for the immune system.” There is growing evidence that it might play a role in autoimmune diseases, in which the immune system mistakenly attacks the body’s own tissues and organs. The Th17 cells and M1 macrophages that became more prevalent in high-salt environments, for example, are pro-inflammatory immune cells with important functions in the body’s defense – and have also been associated with the development of autoimmune diseases.
In addition to examining pro-inflammatory cells, the scientists took a look at anti-inflammatory immune cells, including an important subgroup of phagocytes called type 2 macrophages. These cells have regulatory and suppressive functions, are responsible for repair processes in the body and play a role in wound healing. “We now asked whether salt has an impact on these cells as well,” says Müller.
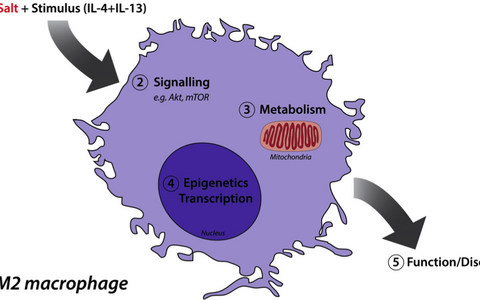
To find out, the international research team, led by Dominik Müller and first authors Katrina Binger and Matthias Gebhardt from the MDC, extracted macrophage precursor cells from the bone marrow of mice and stimulated their development into a type of M2 macrophage. They cultivated some of the cells in petri dishes in a nutrient solution with a high salt content, and another group of cells in petri dishes with normal, low salt concentrations. The results were unequivocal: a high salt environment caused a sharp drop in the activity of M2 macrophages.
To find the mechanism responsible for this effect, the researchers made a comparison of the genes that were activated in the two types of cells in response to salt. They discovered that different genes activate M2 macrophages and pro-inflammatory M1 cells, indicating that salt affects different biochemical pathways.
Finally, Müller’s team studied how too much salt affected immune cells in living animals. Over two weeks the researchers fed one group of mice a low-salt diet, while another group received a diet with high levels of salt. At that point they compared the effects of the diets on wound healing – a process in which M2 macrophages play a crucial role. They discovered delays in wound healing in the mice that had eaten too much salt. The reason for this, the researchers suppose, is a reduction in M2 activity.
“This work allowed us to demonstrate that salt impairs the suppressive and regulatory functions of the immune system," Müller says. The findings are supported by another study, headed by David Hafler of Yale University in New Haven, that is being published concurrently in the Journal of Clinical Investigation. Hafler's team has established that salt affects not only M2 macrophages, but also the functions of anti-inflammatory T cells called Tregs.
“The important finding is that salt pushes the immune system out of equilibrium,“ Müller explains. The effects on macrophages fall along a spectrum – at one end we find pro-inflammatory cells such as the M1 macrophages, whose activity increases with too much salt, and at the other extreme anti-inflammatory M2 macrophages, whose activity decreases.
“When you combine the results of our previous studies with the current work, what you see is that too much salt tilts the balance in favor of pro-inflammatory cells,“ Müller says. This strengthens a long-held suspicion that the high salt diet of industrialized countries, in combination with genetic and other factors, might be partly responsible for the increase of autoimmune diseases such as multiple sclerosis and psoriasis observed over the past few decades. Müller and his team will study in more detail the ways salt confuses the immune system.
Highlight Reference:
High salt reduces the activation of IL-4+IL-13 stimulated 1 macrophages
Binger, K.J., Gebhardt, M., Heinig, M., Rintisch, C., Schroeder, A., Neuhofer, W., Hilgers, K., Manzel, A., Schwartz, C., Kleinewietfeld, M., Voelkl, J., Schatz, V., Linker, R.A., Lang, F., Voehringer, D., Wright, M.D., Hübner, N., Dechend, R., Jantsch, J., Titze, J., Müller, D.N.
J Clin Invest. 2015;125(11):4223–4238. doi:10.1172/JCI80919.
Read the MDC Press Release