In severe COVID-19, neutrophils work overtime
Joint press release of BIH and Max Delbrück Center
Our study shows just how powerful the combination of single-cell technologies and state-of-the-art bioinformatics analysis can be when it comes to investigating complex diseases and their complications, such as the severe lung inflammation caused by COVID-19.
Anyone seeking to positively influence SARS-CoV-2 progression needs information about the early phase of infection. Studies on patients who have already contracted COVID-19 occur too late in the disease process – unlike studies in animal models. Using single-cell analyses, Dr. Samantha Praktiknjo of the Berlin Institute of Health at Charité (BIH), the labs of Professor Markus Landthaler of the Max Delbrück Center and Professor Jakob Trimpert of Freie Universität Berlin as well as researchers at Charité – Universitätsmedizin Berlin were able to track over time what happens from the onset of infection to organ damage in humans and hamsters. The key players at the cellular level are neutrophils (immune cells) and endothelial cells (blood vessel lining cells), as the groups write in “Cell Reports.”
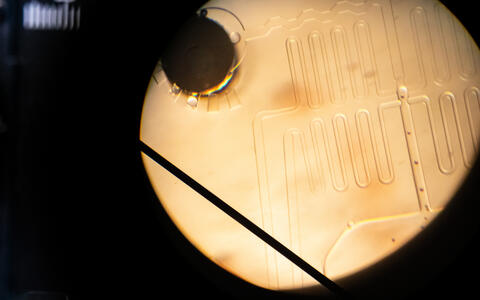
“Using single-cell RNA analyses, we can collect data on gene expression in many individual cells and observe the molecular biological processes as the infection progresses,” explains Samantha Praktiknjo, a researcher at the Berlin Institute of Health at Charité and one of the co-last authors of a newly published study.
“Our study shows just how powerful the combination of single-cell technologies and state-of-the-art bioinformatics analysis can be when it comes to investigating complex diseases and their complications, such as the severe lung inflammation caused by COVID-19,” says Markus Landthaler, who is also a co-last author of the study.
Single-cell sequencing of lung samples
The scientists systematically compared data obtained from human COVID-19 studies, including bronchoalveolar lavage and nasal swabs and post-mortem examinations of lung tissue, with the data obtained from the animal model before evaluating their relevance for humans. Hamsters have proven to be a suitable animal model for COVID-19, as they can be readily infected with the same SARS-CoV-2 variants as humans and show a similar disease pattern. Using single-cell RNA sequencing, the researchers examined lung biopsies from healthy and infected animals at different time points after infection. They compared the dynamic cellular and molecular processes in two different hamster species: the golden or Syrian hamster, which shows a moderate course of COVID-19, and the Roborovski dwarf hamster, which normally experiences severe disease progression.
Single-cell RNA sequencing can be used to find out which sections of genetic information were activated in the cells at the time of sampling. This enabled them to gain an overview of what’s happening in the different cells of tissue samples.
Research in recent years has shown that the aggressive nature of the virus is not the only factor responsible for severe courses of COVID-19 infection. The inflammatory response of the host organism also plays a role. Inflammation is a vital defense mechanism that protects the body from pathogens and is completely normal. But when inflammation goes into overdrive and releases large quantities of pro-inflammatory signaling molecules, it can cause damage to various organs.
Severe disease course is set early on
What determines whether the disease will take a severe course in a patient had previously been unclear, as had the question of when exactly this course is set. "With the help of in-depth single-cell RNA-sequencing analysis and novel machine learning methods we were able to characterize cell activity from the moment of infection", says BIH scientist Samantha Praktiknjo.
Our studies confirm and expand the findings on the role of excessive immune and inflammatory responses in COVID-19.
They identified two distinct patterns of gene activation in the animal model. In both moderate and severe cases of COVID-19, neutrophil granulocytes (or neutrophils), which belong to the first line of defense of the innate immune response, are activated shortly after infection. In moderate cases, the neutrophils are activated for a brief period of time, but then other immune cells like natural killer cells (type 1 immune response) take over. In severe cases, however, the neutrophils remain permanently activated (type 3 immune response), leading to a “storm” of pro-inflammatory signals and massive inflammatory responses in the lungs.
A hallmark of severe COVID-19 progression is damage to the endothelium (the lining of the blood vessels) across multiple organs. In both hamster species, the researchers found strong activation of the vascular endothelium of the lungs, which induced neutrophils to release pro-inflammatory signals. In the Roborovski hamster this resulted in severe endothelial damage, but in the golden hamster the endothelial cells reverted to ground state without incurring significant damage. “Our methodology has allowed us to document, for the first time, the crucial role that endothelial cells play in the development of a severe disease course,” says Dr. Stefan Peidli, one of the first authors of the study.
“Our studies confirm and expand the findings on the role of excessive immune and inflammatory responses in COVID-19,” adds Praktiknjo. “We will continue our research in this direction and hope to identify targets for innovative therapies that can be used to steer the infection process along the right path early on.”
Text: BIH
Further information
Literature
Stefan Peidli, Geraldine Nouailles et al. (2024): “Single-cell-resolved interspecies comparison shows a shared inflammatory axis and a dominant neutrophil-endothelial program in severe COVID-19.” Cell Reports, DOI: https://doi.org/10.1016/j.celrep.2024.114328
Contacts
Konstanze Pflüger
Head of Communications
Berlin Institute of Health in der Charité (BIH)
+49 (0)30 450 543 343
pressestelle-bih@bih-charite.de
Jana Schlütter
Editor, Communications
Max Delbrück Center
+49 30 9406-2121
jana.schluetter@mdc-berlin.de or presse@mdc-berlin.de
- Max Delbrück Center
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (Max Delbrück Center) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the locations in Berlin-Buch and Mitte, researchers from some 70 countries study human biology – investigating the foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium of a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should be able to benefit as soon as possible from basic research discoveries. This is why the Max Delbrück Center supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly-run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the Max Delbrück Center today employs 1,800 people and is 90 percent funded by the German federal government and 10 percent by the State of Berlin.