Preeclampsia: Inflammation of the placenta interferes with fetal development
In the womb, the fetus receives the nourishment it requires via the placenta. It is here that the blood vessels of the mother and the unborn child meet, without the blood itself mixing. If the formation of the placenta is disrupted, preeclampsia can occur – a disorder affecting the mother that is characterized by high blood pressure, water retention and protein in the urine. It can also impact the growth of the fetus.
“Even after many years of research, the clear causes and mechanisms of preeclampsia remain unknown,” says Berlin-based researcher Dr. Florian Herse. “This is why one of its nicknames is ‘the disease of theories’”
Herse is a scientist in the working group of Prof. Dominik N. Müller and Dr. Ralf Dechend at the Experimental and Clinical Research Center (ECRC) and the Berlin Institute of Health (BIH). These two institutions bring together researchers from the Max Delbrück Center for Molecular Medicine (MDC) in the Helmholtz Association and Charité – Universitätsmedizin Berlin. In a new study published in the journal Circulation Research, Herse and his international research team have now identified a factor in the immune system that is relevant for the disorder.
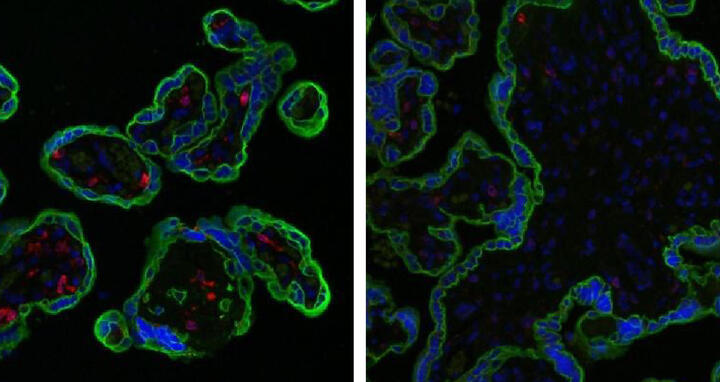
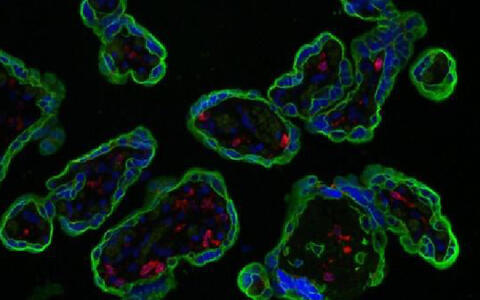
The deciding factor is the presence of receptor protein CD74, which is found on the surface of immune cells. In the placenta, the researchers found this protein on the large phagocytes, known as macrophages, that form part of the immune system. These cells are active at the interface between mother and child; they interact directly with and stimulate other placental cells – namely the trophoblasts.
“In preparatory studies, we noticed that the presence of CD74 was lower in the placentas of preeclamptic women,” says Herse. The researchers therefore decided to investigate this correlation more closely. In so doing, they discovered that there were far fewer CD74 receptors on the placental macrophages of the affected women than expected. In a cell culture test, the researchers suppressed the production of CD74 in the macrophages, which resulted in pro-inflammatory substances being released. The placentas of mice without the CD74 protein had abnormal structural features and had a lower performance than those of the control group.
The researchers believe that the direct cause of the inflammation and the abnormal appearance of the placentas lies in disrupted communication between cells. “The reason for the disturbed placental growth is the disruption of the macrophage-trophoblast interaction, which is important for a normal pregnancy,” says Herse, summarizing the findings.
Herse explains that the comprehensive methodology makes the results particularly robust, and that the study provides sound evidence of a correlation between the receptor protein and the disease: “We followed a translational research approach using human test subjects, cell culture experiments, and animal models.”
However, exactly why lower quantities of the CD74 receptor are produced in affected women and how this triggers the disorder’s many symptoms is still unknown. On these points, the researchers can only speculate.
“The association between CD74 receptors and preeclampsia opens up new long-term possibilities for developing a much-needed therapy that targets the root causes rather than the symptoms of the disease,” says Herse. Despite decades of research, such a therapy does not yet exist.
This work was funded by the German Research Association (DFG). First author Lukasz Przybyl, PhD student in the MDC Transcard Program, got his PhD with this work.
Lukasz Przybyl1,3, Nadine Haase1,2,3, Michaela Golic1,3,4, Julianna Rugor1,3, Maria Emilia Solano5, Petra Clara Arck5, Martin Gauster6, Berthold Huppertz6, Christoph Emontzpohl7, Christian Stoppe7,8, Jürgen Bernhagen7,9,10, Lin Leng11, Richard Bucala11, Herbert Schulz3,12, Arnd Heuser2, M. Susanne Weedon- Fekjær13,14, Guro M. Johnsen13,14, Dirk Peetz15, Friedrich C Luft1,2, Anne Cathrine Staff13,14, Dominik N Müller1,2,3, Ralf Dechend1,3,15 Florian Herse1,2,3 (2016): „CD74-Downregulation of Placental Macrophage-Trophoblastic Interactions in Preeclampsia.“ Circulation Research (published online first at May 19 2016). doi:10.1161/CIRCRESAHA.116.308304
1Experimental and Clinical Research Center, a joint cooperation between the Max-Delbrück Center for Molecular Medicine in the Helmholtz Association and the Charité Medical Faculty, Berlin, Germany; 2Max-Delbrück Center for Molecular Medicine in the Helmholtz Association, Berlin, Germany; 3Berlin Institute of Health (BIH), Berlin, Germany; 4Charité Universitätsmedizin Berlin, Departments of Obstetrics, Gynecology, and Senology, Charité Campus Mitte, Berlin, Germany; 5Department of Obstetrics and Fetal Medicine, Laboratory for Experimental Feto-Maternal Medicine, University Medical Center Hamburg- Eppendorf, Germany; 6Institute of Cell Biology, Histology and Embryology, Medical University of Graz, Austria; 7Institute of Biochemistry and Molecular Cell Biology, RWTH Aachen University, Germany; 8Department of Anesthesiology, RWTH Aachen University, Germany; 9Vascular Biology, Institute for Stroke and Dementia Research, Klinikum der Universität München, Ludwig-Maximilians-University, 81377 Munich, Germany; 10Munich Cluster for Systems Neurology (SyNergy), 81377 Munich, Germany; 11Department of Internal Medicine, Yale University School of Medicine, New Haven, Connecticut, USA; 12Cologne Center for Genomics (CCG), University of Cologne, Germany; 13Departments of Obstetrics and Gynaecology, Oslo University Hospital, Ulleval, Norway; 14University of Oslo, Norway, and; 15HELIOS-Klinikum, Berlin, Germany.
CD74 (red) is expressed by healthy makrophages (left) and is almost completely diminished in preeclamptic makrophages (right) at the end of pregnancy. Trophoblasts are stained in green. Image: Florian Herse/MDC
Contact
Vera Glaßer
Max Delbrück Center for Molecular Medicine (MDC) Berlin-Buch
Head of Communications department (interim)
Tel: 030/94 06 - 2120
presse@mdc-berlin.de