Multiple myeloma: Early detection of aggressive tumors
Joint press release of Charité, BIH at Charité, and the Max Delbrück Center
Multiple myeloma is one of the most common forms of cancer of the immune cells in the bone marrow. Despite advances in treatment and the introduction of new cellular immunotherapies, there is no cure at present. Even when patients respond to treatment at first, the cancer comes back. To be able to intervene faster and on a more targeted basis, a researchers led by Professor Jan Krönke from the Department of Hematology, Oncology and Cancer Immunology at Charité – Universitätsmedizin Berlin, and Dr. Philipp Mertins, head of the Proteomics technology platform of the Max Delbrück Center and the Berlin Institute of Health at Charité (BIH), teamed up with other partners for a comprehensive study of this disease at the molecular level. They now describe how highly aggressive types of tumors can be detected early on in an article published in the journal “Nature Cancer.” They show how changes in genetic material affect the protein profile of the tumor cells, and thus the mechanisms involved in the disease.
In multiple myeloma, the immune cells in the bone marrow, known as plasma cells, mutate and become cancerous. Plasma cells are responsible for producing antibodies. All humans have many different kinds of plasma cells that form large numbers of different antibodies. This allows the body to recognize and fight various pathogens. In multiple myeloma, a single plasma cell mutates into a tumor cell. That cell reproduces unchecked, forming a monoclonal cell population. This means many cells are formed, all of them exactly the same and genetically identical at first. The mutated cells often also produce large volumes of antibodies or fragments of them – but they do not function properly. Over the course of the disease, most patients develop tumors at various locations in the bone marrow, hence the “multiple” in the disease’s name. Immunodeficiency, kidney failure, bone loss, and bone fractures are just some of the consequences of this uncontrolled cell growth.
What path does the tumor take?
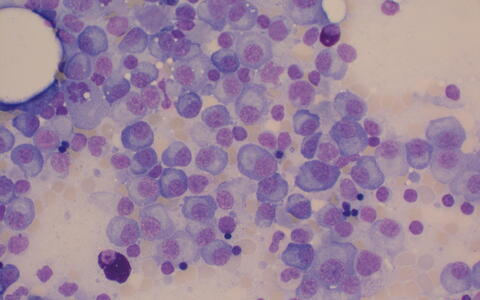
Microscope image of bone marrow with multiple myeloma cells.
No two cases of cancer are alike, and multiple myeloma is no exception. Tumors develop differently in different individuals, including at different rates. This makes it more difficult to predict how the disease will progress and choose the optimum treatment. While the mutated plasma cells do not spread much in some cases, in others they are extremely aggressive, leading to a poor prognosis.
But what causes so much divergence in the course of multiple myeloma? In cooperation with protein analysis experts from the Max Delbrück Center and BIH, the researchers conducted a detailed study of genetic and molecular changes occurring in the tumor cells in a group of more than one hundred patients. The study included data from patients in the German Multiple Myeloma Study Group (DSMM), which is coordinated by the University Hospital of Würzburg. This allowed the researchers to include clinical data on patients who had received standardized treatment over a period of eight years or more following initial diagnosis.
Systems medicine and big data
We wanted to know the consequences of genetic changes at the protein level and compare this molecular biology data against the actual course of the disease in patients.
While changes in the genome and their effects on the proteome are already well described for other types of cancer, this is the first detailed proteo-genomic study of multiple myeloma. “Genetic data alone is insufficient to explain the mechanisms involved in this disease,” Mertins says. “We wanted to know the consequences of genetic changes at the protein level and compare this molecular biology data against the actual course of the disease in patients.” The team was supported in collecting and analyzing the large volumes of data by experts at Charité, BIH, and the German Cancer Consortium (DKTK).
Cutting-edge mass spectrometry methods made it possible to map the protein profile of mutated plasma cells and compare it against that of healthy plasma cells in people without the disease. The researchers found that both genetic changes and changes in signaling pathways lead to uncontrolled activation of cancer cells. Regulatory processes at the protein level had the stronger influence. The researchers identified a protein constellation that suggests the disease will take a particularly aggressive course, regardless of other known risk factors.
Unlocking new therapies
“Our findings will help subcategorize patients more effectively going forward, personalizing their treatment,” Krönke concludes. “We’ve identified key proteins and signaling pathways that can serve as the basis for even more effective, better tolerated treatments for multiple myeloma, for example for immune therapies such as CAR T-cell therapy.” In further steps, the researchers plan to study which of the target structures they have identified are in fact good candidates for new therapeutic approaches.
The study is a crucial resource for research and applied development, says Dr. Evelyn Ramberger, first author of the study: “To make the complex data set manageable, we programmed an interactive, freely available online tool.” This has given cancer researchers easy access to the results, so they can use the information to develop new therapies and tests to help guide treatment. For example, it may be possible to treat patients with an especially aggressive form of multiple myeloma with more intensive therapies right at the outset.
Text: Charité
- Mass spectrometry
Mass spectrometry is a technique for analyzing the mass of molecules and atoms. The substance to be analyzed is ionized and converted to a gas phase. The ions formed are sharply accelerated using an electric field and then sorted by mass-to-charge ratio in the mass spectrometer’s analytical unit. The mass spectrum of a substance provides information on its molecular composition. Mass spectrometry is therefore useful for identifying, characterizing, and quantifying a large number of biomolecules, such as proteins, metabolites, sugars, and fats, which may behave differently depending on the disease and the individual organism.
- About the study
The study was supported by the German Cancer Consortium (DKTK), the German Research Foundation (DFG), the German Federal Ministry of Education and Research (BMBF), the Research Cores for Mass Spectrometry in Systems Medicine (MSCoreSys) research consortium, the Wilhelm Sander Foundation, and Berliner Krebsgesellschaft e.V. In addition to researchers from Charité, the Berlin Institute of Health at Charité (BIH), and the Max Delbrück Center, experts from the German Cancer Research Center (DKFZ) and the University Hospitals of Würzburg and Ulm, and the German Multiple Myeloma Study Group (DSMM: coordination: Professor Stefan Knop and Professor Hermann Einsele), were all instrumental in contributing to the work.
Further information
- Medical Clinic with a focus on Hematology, Oncology and Cancer Immunology at Charité – Universitätsmedizin Berlin (CBF, German)
- Why multiple myeloma returns
- Joint press release of Charité and Max Delbrück Center on MSTARS
Literature
Evelyn Ramberger et al. (2024): “The proteogenomic landscape of multiple myeloma reveals insights into disease biology and therapeutic opportunities.” Nature Cancer, DOI: 10.1038/s43018-024-00784-3
Photos for download
Mass spectrometry makes it possible to create a detailed protein profile of the cancer cells. Shown here is the ion source of a liquid chromatography–mass spectrometry (LC–MS) system. A thin glass tip is used to transfer the specimen being analyzed to the opening of the mass spectrometer. Photo: Pablo Castagnola l Max Delbrück Center
Microscopic image of bone marrow with multiple myeloma cells. Photo: Jan Krönke l Charité
Contacts
Prof. Dr. Jan Krönke
Department of Hematology, Oncology and Cancer Immunology
Campus Benjamin Franklin
Charité – Universitätsmedizin Berlin
Tel. +49 30 450 513 382
jan.kroenke@charite.de
Dr. Philipp Mertins
Head of the Proteomics Platform
Max Delbrück Center
Berlin Institute of Health at Charité (BIH)
Philipp.Mertins@mdc-berlin.de
Jana Schlütter
Editor, Communications
Max Delbrück Center
+49 30 9406-2121
jana.schluetter@mdc-berlin.de or presse@mdc-berlin.de
- Max Delbrück Center
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (Max Delbrück Center) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the locations in Berlin-Buch and Mitte, researchers from some 70 countries study human biology – investigating the foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium of a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should be able to benefit as soon as possible from basic research discoveries. This is why the Max Delbrück Center supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly-run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the Max Delbrück Center today employs 1,800 people and is 90 percent funded by the German federal government and 10 percent by the State of Berlin.