Simon Lab
Cell Biology of Immunity
Profile
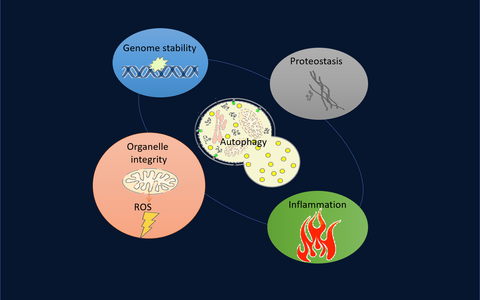
Cells are specialists in sustainability. They eat up all the organelles or larger molecular complexes that they no longer need – in order to then recycle the digestion products to build new structures. Autophagy is the name of this cellular recycling process, which yeast, but also all plant, animal and human cells use for themselves. Without autophagy, cells cannot develop and function normally, they age faster without it, and so does the immune system. In our lab we investigate the role of autophagy in the immune system and how to use autophagy to keep the immune system young.
Team
Research
Autophagy is a major degradation pathway in the cell. While the ubiquitin/proteasome system degrades proteins, autophagy degrades bulk cytoplasmic material. Autophagosomes have been shown to engulf whole organelles, such as mitochondria, lipid droplets and ER and as a consequence autophagy impacts on metabolism, apoptosis, differentiation, cell cycle and cell fate decisions in the cell.
Over the last decade we have studied the role of autophagy in the development and function of hematopoietic and immune cells using in vivo models and in vitro techniques applied to human samples.
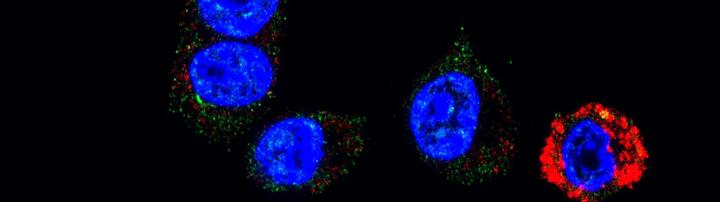
We pioneered a technique detecting autophagy in primary cells and showed a decrease in autophagy levels in ageing T lymphocytes (Phadwal et al, Autophagy 2012). Our research also revealed that red blood cells need autophagy to degrade mitochondria for their final maturation (Mortensen et al, PNAS 2010). Hematopoietic stem cells require autophagy for their maintenance (Mortensen, J Exp Med et al, 2011), and in the absence of autophagy, we observe a mild pre-leukemic phenotype. We measured low levels of autophagy in human acute myeloid leukemia samples (Watson et al, Cell Death Discovery 2015). Autophagy is required for neutrophil differentiation by providing free fatty (Riffelmacher et al, Immunity 2017). We also found that B2 cells require autophagy for self-renewal and their specific metabolism for survival, but not B1 cells (Clarke et al, JEM 2018). The survival/ maintenance of memory T cells is also reliant on autophagy. We find that inducing autophagy in T cells from aged donors with spermidine, an endogenous metabolite and polyamine, reverses an inefficient memory T cell response to influenza vaccination (Puleston et al, elife, 2014). Downstream of polyamines we have discovered a novel pathway that controls autophagy translationally, and is decreased with age. Re-introducing autophagy also improves B cell responses in older mice and adults. (Zhang et al, Mol Cell 2019, Alsaleh et al, elife 2020). Together these findings formed the basis for a clinical trial that aims at improving vaccine responses with polyamines with a particular focus on halting the waning of memory responses in older adults (https://clinicaltrials.gov/ct2/show/NCT05421546).
We are now trying to understand the role of autophagy in immune cell fate mechanistically, by identifying the autophagosomal cargo in vivo with a novel proximity labelling mouse model (Zhou et al, Nat Comms 2022). Furthermore we want to know whether and how autophagy in the microenvironment impacts on immune cells (Richter et al, biorxive 2022) and what autophagy provides to hematopoietic stem cells (Borsa, Obba et al. submitted). With this knowledge we are aiming to identify novel drug targets and drugs to be used for hematopoietic malignancies, in regenerative medicine and vaccination of older adults.