Detonating fuse for breast cancer discovered
Breast cancer is the most common type of tumour found in women. 69,000 new cases are diagnosed each year in Germany alone. Around 80 percent of tumours originate in the luminal cells, the milk-producing cells of the mammary gland. 10 percent of the cells resemble those of the underlying (basal) cell layer. These are muscle-like epithelial cells that contract when the mammary gland produces milk in order to push it out.
We do not see any breast tumours in the absence of YAP. YAP is therefore required for the development and spread of the tumour.
“While luminal breast tumours are usually sensitive to hormones, 80 percent of basal-like tumours are triple-negative. They have no receptors for estrogen (ER), progesterone (PR) or the growth factor receptor HER2”, says Professor Walter Birchmeier. He heads the Signal Transduction in Development and Cancer Lab at the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC). As there are currently no targeted treatments for this very aggressive form of cancer, the prognosis for affected patients is poor. These tumours rarely respond to conventional chemotherapeutic agents, which are intended to inhibit cell division.
The tumours did not grow in the mice in the absence of YAP
In previous studies, Birchmeier’s team was able to demonstrate that the Wnt/β-catenin pathway plays a key role in the development of basal-like breast cancer. This signalling cascade normally regulates cell proliferation and differentiation during embryonic development. Wnt is essential for the β-catenin protein to signal to the nucleus. Once the cells are mature and ‘the job has been done’, this reaction chain is disabled and β-catenin is degraded. However, the signalling pathway can be reactivated in some types of cancer. In the case of basal-like breast cancer, it is activated and β-catenin accumulates in the tumour cells. It was also known that the YAP oncogene is upregulated in cancer stem cells. The YAP protein stimulates cell growth and is also active in the nucleus.
The aim of the current study was to investigate the connection between Wnt signalling and YAP. PhD student Hazel Quinn, lead author of the study, deactivated the YAP gene at the onset of tumour growth in mice in which the Wnt signalling pathway was activated and basal-like breast cancer was induced. It was found that while mice in the control group developed massive tumours within weeks, this did not occur in the YAP knockout mice.
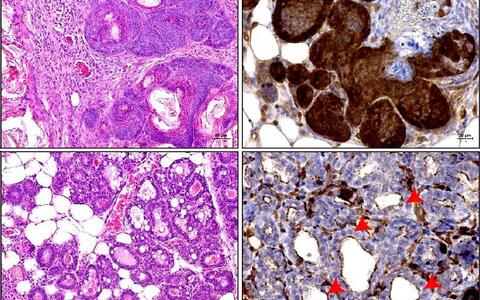
“We do not see any breast tumours in the absence of YAP. YAP is therefore required for the development and spread of the tumour,” says Hazel Quinn The scientist used dyes and specific antibodies to make YAP in the nuclei visible in tissue sections. The alveoli – small sack-like structures in which the milk is formed and stored – are easily recognisable and free of tumours when the YAP gene is deactivated. They are almost invisible in the tissue of the control group because the proliferating carcinoma displaces them.
Conclusions regarding survival
YAP is a key regulator in the Hippo signalling pathway, which was only discovered a few years ago. It plays an important role in cell regeneration and differentiation for stem cells. If it does not function correctly, cancer can develop. “It is also likely to be the reason why the YAP gene is highly expressed in basal-like breast cancer but not in luminal breast cancer. The cells of basal-like tumours are similar to stem cells, whereas luminal tumours are much more differentiated,” explains Hazel Quinn.
Head of proteomics platform
Quinn’s co-author Dr. Philipp Mertins, expert in proteomic analysis and group leader at MDC and the Berlin Institute of Health (BIH), carried out gene expression analyses on tissue samples from human breast tumours and was able to confirm this hypothesis. While basal-like tumours generally exhibit high expression levels of the YAP gene, these are significantly lower in luminal breast cancer. How much YAP is present in the tumour is also directly correlated with the survival time of patients. “The higher the YAP level in triple-negative breast cancer, the earlier women died. In the case of luminal breast cancer, the reverse is true,” explains Hazel Quinn.
Approach to targeted therapy
Cancer stem cells are usually the reason why small tumour clusters remain in the tissue despite chemotherapy, and the cancer returns at a later stage and forms metastases. Unlike in mice, genes in humans cannot simply be deactivated. However, the good news is that YAP can be inhibited with medication. “As we now know how important YAP is for these cells, the combination of YAP inhibitors that do not produce any non-specific side effects and conventional therapeutic strategies could improve patients’ chance of survival without recurrence,” says Hazel Quinn.
Combination treatments with different inhibitors that work at different points of signalling pathways are currently being favoured.
Quinn demonstrated that this could be done in mice by inhibiting YAP activity with the substances Simvastatin or Verteporfin, which are approved for treating other diseases. Both inhibitors significantly reduced the tumour volume. “A German pharmaceutical company is currently researching molecules that can specifically inhibit YAP,” adds Walter Birchmeier. It may be some time before a highly effective and well-tolerated new active ingredient is discovered and can be used in the clinic. “Combination treatments with different inhibitors that work at different points of signalling pathways are currently being favoured,” says Birchmeier.
Text: Catarina Pietschmann
Further information
Literature
Hazel Quinn et al. (2021): „YAP and b-catenin cooperate to drive oncogenesis in basal breast cancer“. Cancer Research, DOI: 10.1158/0008-5472.CAN-20-2801
Download
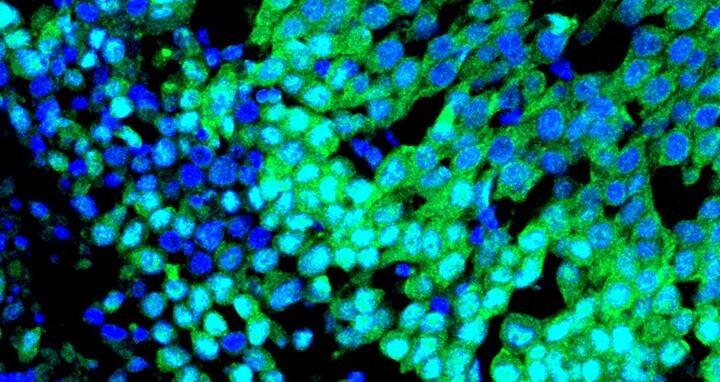
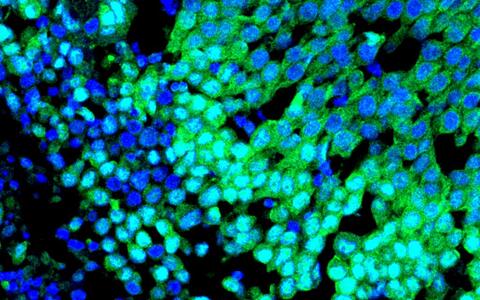
Immunofluorescence image of a patient derived xenograft (PDX) basal breast tumour showing strong nuclear localisation of the oncogenic protein YAP (green) and nuclei (blue). © Birchmeier Lab
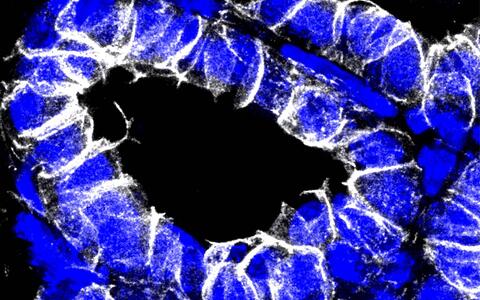
Immunofluorescence image of the post-partum mouse mammary gland showing membrane bound B-catenin (white) and nuclei (blue). © Birchmeier Lab
Contacts
Prof. Walter Birchmeier
Signal Transduction in Development and Cancer
Max Delbrück Center for Molecular Medicine in der Helmholtz Association (MDC)
Tel.: +49-30-941 43 48
wbirch@mdc-berlin.de
Hazel Quinn, PhD
Brisken Laboratory
Swiss Institute of Experimental Cancer Research, Lausanne
Mobil +41(0) 7 79 91 70 02
hazel.quinn@epfl.ch
Jana Ehrhardt-Joswig
Editor, Communications Department
Max Delbrück Center for Molecular Medicine in der Helmholtz Association (MDC)
jana.ehrhardt-joswig@mdc-berlin.de oder presse@mdc-berlin.de
- The Max Delbrück Center for Molecular Medicine (MDC)
-
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the MDC’s locations in Berlin-Buch and Mitte, researchers from some 60 countries analyze the human system – investigating the biological foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium in a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should benefit as soon as possible from basic research discoveries. The MDC therefore supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the MDC today employs 1,600 people and is funded 90 percent by the German federal government and 10 percent by the State of Berlin.