Restoring the elasticity of heart muscle
Sometimes, the human heart struggles to pump blood throughout the body. There are myriad causes, but one of the most common is a condition called heart failure with preserved ejection fraction (HFpEF) – particularly among older adults. In HFpEF, the heart’s pumping power remains intact, but its muscle becomes stiff with age, making it harder for the organ to fill effectively with blood. There is no effective treatment.
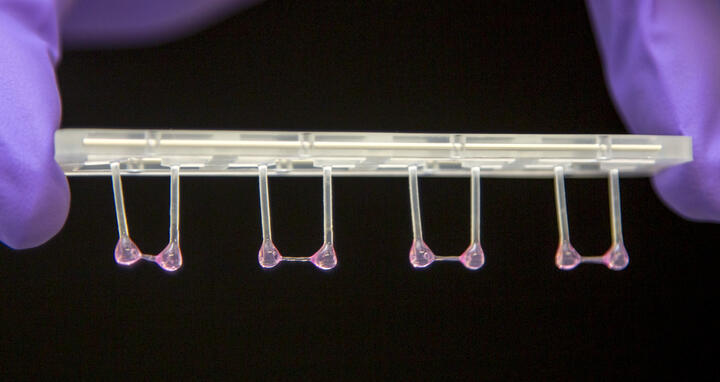
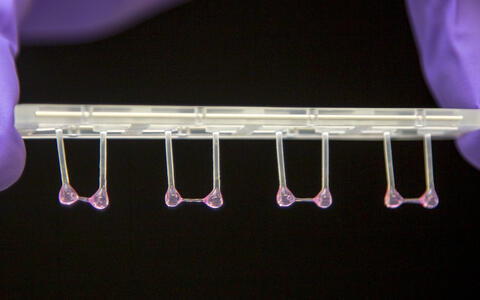
Artificial heart tissue can contract against a resistance and then relax.
Professor Michael Gotthardt, Group Leader of the Translational Cardiology and Functional Genomics lab at the Max Delbrück Center, is developing a therapy to restore the heart’s lost flexibility. “We’ve already shown in animal models and in human heart tissue derived from stem cells that this is possible,” he says. “We had to get heart muscle cells to produce more of the flexible version of the protein titin, similar to what happens early in life.”
To bring this approach to patients with HFpEF as quickly as possible, the Deutsche Zentrum für Herz-Kreislauf-Forschung (DZHK) is providing over €650,000 in funding over the next four years. Gotthardt submitted the proposalwith clinical partner Dr. Alessio Alogna from the Deutsches Herzzentrum der Charité (DHZC), with whom he will share the grant. The two researchers have named their project SMASH, short for “Splice Modulation Approach to Suppress HFpEF.”
Targeted delivery to the heart
Gotthardt and Alogna’s approach uses antisense oligonucleotides (ASOs) – short, single-stranded molecules of nucleic acid. These molecules reduce the amount and activity of a splicing factor called RBM20. This factor plays a key role in determining whether the body produces flexible or stiff versions of titin, a giant protein that acts like a spring within the heart muscle. “With our ASOs, we were able to completely reverse stiffened hearts and HFpEF symptoms in mice,” says Gotthardt.
With our ASOs, we were able to completely reverse stiffened hearts and HFpEF symptoms in mice
But the approach still has one major drawback: side effects. “In animal models, it caused an enlarged spleen and immune system disturbances,” Gotthardt explains. With the DZHK funding, he now aims to modify the ASOs so that they target only the heart, specifically heart muscle cells, and avoid organs like the liver. “It’s basically a matter of the right packaging,” he says.
Gotthardt also wants to show that the modified ASOs also work in human heart tissue. For this, he and his team will use engineered heart tissue grown from human stem cells – structures that expand and contract like real hearts.
Preparing for human trials
“To eventually test ASOs in patients, we also need to demonstrate their clinical benefit in a second animal model,” Gotthardt explains. That’s where his colleague Alogna comes in. Using the newly approved funds, the cardiologist will lay the groundwork for future studies in a porcine model of HFpEF, and Gotthardt will provide the necessary ASOs to test whether they can restore elasticity in pig hearts as well.
Text: Anke Brodmerkel