The ebb and flow of brain ventricles
It is not only the heart that has chambers – the brain does, too. Its four ventricles are connected to the spinal canal and filled with a clear liquid called cerebrospinal fluid, which removes metabolic waste from the neurons. If the brain becomes inflamed, immune cells also circulate in this fluid. This is the case in diseases like multiple sclerosis (MS), where the immune system attacks the body’s own protective layer around axons (nerve fibers) in the brain and spinal cord. This triggers inflammation, which ultimately leads to the destruction of neurons.
Usually, the brain’s ventricle volume remains fairly constant. However, in 2013, Dr. Sonia Waiczies and her colleagues from the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) and Charité – Universitätsmedizin Berlin made a discovery in an MS animal model: They observed that the ventricle volume changed over the course of the disease. When they used an antigen to trigger encephalitis (inflammation of the brain) in mice, MRI scans clearly showed that the ventricles expanded. “Everyone thought it was a sign of brain atrophy,” Waiczies recalls.
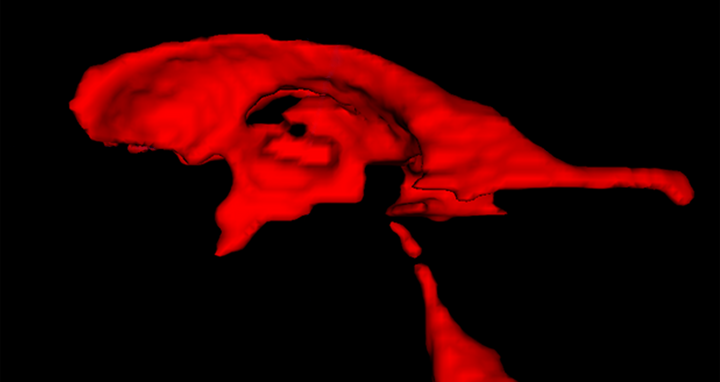
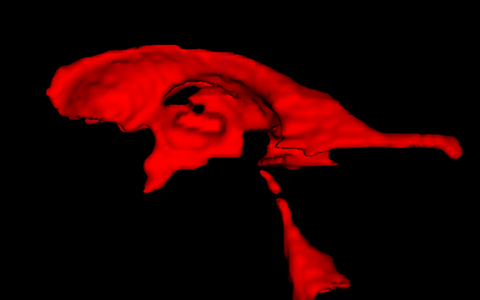
3d rendering of the ventricle volumes from a study participant.
The swelling goes back down
If the brain’s ventricles become larger, it follows that the brain must become smaller. After all, the surrounding skull bone leaves it with nowhere else to go. Inflammation does indeed cause brain tissue damage, but atrophy – i.e., a massive loss of brain volume –
does not always occur immediately . And if it did, this process would be non-reversible. “So we conducted a series of further animal experiments, and monitored the brain volumes over two months,” says the neuroimmunologist and senior author of the current study. About ten days after the encephalitis was induced, the rodents’ brain ventricles were significantly enlarged. Then, a few days later, they shrunk back to normal size when the symptoms remitted. Just like the patients, they went on to develop temporary relapses – albeit with milder symptoms than at first – and the ventricles would again become enlarged.
If I have an inflamed joint, for example, an edema forms and it swells up. Once the inflammation subsides, the swelling also goes down.
Waiczies, who also works as an MR scientist, finds these results quite logical: “If I have an inflamed joint, for example, an edema forms and it swells up. Once the inflammation subsides, the swelling also goes down.” The team is interested in the molecular mechanisms behind these changes. But first, they wanted to know whether their findings had clinical relevance.
Archival data confirms new findings
Enlarged brain ventricles in people with MS is commonly thought to be a sign of brain atrophy. A reduction in ventricle size had never been reported in patients. So what does this observation mean for MS patients? And can the finding even be transferred from mice to humans? The current study saw the researchers test this with the help of extensive MRI data sets of MS patients. From 2003 to 2008, they had participated in a clinical trial at the Charité to test the effects of a new MS drug. “I was involved in the immunological planning and evaluation of this study, and I knew that the generated MRI data was extensive and robust,” says Waiczies.
We are used to seeing ventricular enlargement in other neurodegenerative diseases – such as Alzheimer’s or Parkinson’s disease. But in those diseases, rather than being reversible, the ventricles just keep expanding.
A diagnosis of multiple sclerosis is made from MR images and by analyzing cerebrospinal fluid obtained by puncturing the spinal cord. Regular scans allow a better prognosis of disease progression. In this study, participants had received a monthly MRI scan. Countless images now had to be viewed and statistically evaluated. Lead author Dr. Jason Millward, neuroimmunologist at the MDC and Charité and statistics enthusiast, set to work on the new study.
“The key factor was the number of measurements taken over time, which provided us with a unique opportunity to see if the patients exhibited similar trends,” explains Millward. That was indeed the case: “The majority of patients with relapsing-remitting MS exhibited fluctuations in ventricle volume – just as we observed with the mice.” Interestingly, Millward also found that the patients with changes in ventricle volume seemed to be in an earlier stage of the disease.
“We are used to seeing ventricular enlargement in other neurodegenerative diseases – such as Alzheimer’s or Parkinson’s disease. But in those diseases, rather than being reversible, the ventricles just keep expanding,” explains Professor Thoralf Niendorf of the MDC, who also works at the Experimental and Clinical Research Center (ECRC), a joint institution of the MDC and Charité. “Regular monitoring of ventricle volume in MS patients could help to distinguish temporary fluctuations from progressive brain atrophy.” This would also make it possible to better tailor therapies to the individual patient.
From a clinical perspective, examining fluctuations in ventricle volumes in routine MRI patient scans could be an interesting approach to monitoring the course of the disease or of immune therapies.
Professor Friedemann Paul, a clinical neuroimmunologist at Charité and, together with Waiczies and Niendorf, the current study’s senior author, adds: “From a clinical perspective, examining fluctuations in ventricle volumes in routine MRI patient scans could be an interesting approach to monitoring the course of the disease or of immune therapies. But this will require us to study even larger cohorts over a longer period of time. Comparing these results with clinical findings – for example, regarding cognition – is also going to be important.”
The researchers now want to understand how the “ebb and flow” of brain ventricles occurs at the molecular level.
Text: Catarina Pietschmann
Further information
New therapeutic options for multiple sclerosis in sight
Possible therapy for repairing myelin in multiple sclerosis?
Downloads
A 3D view of the brain ventricles of a study participant. Photo: Millward et al., MDC
Literature
Sonia Waiczies, Jason M. Millward et al. (2020): „Transient enlargement of brain ventricles during relapsing-remitting multiple sclerosis and experimental autoimmune encephalomyelitis“, JCI Insight, DOI: 10.1172/jci.insight.140040
Contacts
Christina Anders
Editor, Communications Department
Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC)
+49-(0)30-9406-2118
christina.anders@mdc-berlin.de or presse@mdc-berlin.de
Dr. Sonia Waiczies
Fluorine Magnetic Resonance Imaging in Immunology
Experimental Ultrahigh Field Magnetic Resonance Lab
+49-(0)30-9406-4542
sonia.waiczies@mdc-berlin.de
- The Max Delbrück Center for Molecular Medicine (MDC)
-
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the MDC’s locations in Berlin-Buch and Mitte, researchers from some 60 countries analyze the human system – investigating the biological foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium in a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should benefit as soon as possible from basic research discoveries. The MDC therefore supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the MDC today employs 1,600 people and is funded 90 percent by the German federal government and 10 percent by the State of Berlin.