Coronavirus research at the MDC
In a crisis like the present pandemic, Berlin can draw on a wide range of expertise in basic research, clinical science and epidemiology and in highly specialized technologies and infrastructures. “These researchers are now coordinating with each other here in Berlin and with other researchers around the world to pool together resources to investigate SARS-CoV-2. We at the MDC are also contributing to the bigger picture,” says Professor Thomas Sommer, Scientific Director (interim) of the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC).
As of March 18, 2020, the MDC has reduced its operations to a minimum in order to slow the spread of the SARS coronavirus-2 and protect its employees. The scientists are working from home, as are administrative staff, where they are developing ideas, analyzing data, and writing proposals and papers. Regular research activities in the labs have been suspended. Only staff assigned to emergency operations have lab access during this time. Exempted from this rule are projects and technology platforms that advance the understanding of the novel coronavirus or its disease, COVID-19. These activities at the MDC are coordinated by Professor Markus Landthaler.
Several collaborations have been in place for many years. But a number of the MDC’s research labs have shifted their focus because they want to help.
“We are primarily supporting our colleagues at Charité – Universitätsmedizin Berlin,” Sommer says. “Several collaborations have been in place for many years. But a number of the MDC’s research labs have shifted their focus because they want to help.” The pan-European LifeTime consortium, which is jointly coordinated by Nikolaus Rajewsky at the MDC and Geneviève Almouzni at the Institut Curie in Paris, is also using its expertise to study the infection.
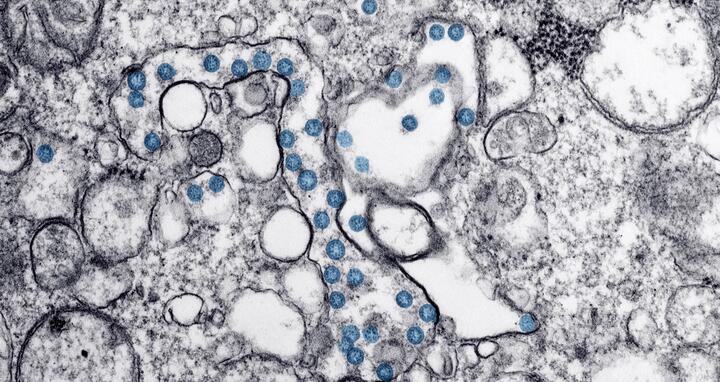
Since there are no biosafety level 3 laboratories at the MDC, the researchers are working exclusively with inactivated viruses or samples in which the virus is no longer present. Here’s an overview of the MDC’s current collaborations and plans.
How does the infection affect individual cells?
When the lungs become inflamed due to a SARS-CoV-2 infection, all cells do not respond in the same way to the disease. In the lungs, as in other organs, there are a wide variety of cells packed closely together. Each of these cell types is present in different cell states, and they are infected to varying degrees by the virus and undergo changes as COVID-19 progresses.
This heterogeneity can be characterized in detail using single-cell sequencing technologies and other high-throughput methods – at the mRNA level for human cells and viral RNA and at the protein level. A single sample generates millions of data points about the molecular consequences of the infection, which are then analyzed with the aid of computational methods. This allows scientists to investigate questions such as: What signaling pathways are activated? What distinguishes the new SARS virus from earlier strains? How precisely does the virus replicate, and what type of cellular immune response does this elicit?
“The first aim of the experiments is to establish a better basic understanding of this still largely unknown virus and compare it with other coronaviruses,” says Professor Matthias Selbach, head of the Proteome Dynamics Lab at the MDC.
At Charité – Universitätsmedizin Berlin, scientists have already infected lung epithelial cell lines with the novel coronavirus. The plan is to do the same with pieces of human lung tissue, human lung organoids, brain organoids (to study how the nervous system is affected) and cardiomyocytes (to study how the heart is affected) that were grown from induced pluripotent stem cells. Such cell culture systems allow the scientists to spatiotemporally observe the progression of the infection and its effects. In addition, the LifeTime consortium has set up a coronavirus task force to push this research forward in collaboration with partners across Europe.
“The ultimate goal is to identify highly specific molecular target structures that are medically relevant,” says Professor Nikolaus Rajewsky, Scientific Director of the MDC’s Berlin Institute for Medical Systems Biology (BIMSB) and head of the Systems Biology of Gene Regulatory Elements Lab. Among other activities, his lab is developing new methods to measure gene expression in 3D in tissues. “This enables us to see which cell types are infected, how different cells react to the infection or to the treatment, and which molecules play an important role,” Rajewsky explains. “These are all avenues for improving diagnostics and therapeutics.”
Dr. Emanuel Wyler from the Landthaler Lab uses single-cell sequencing to study how the new SARS virus differs from older strains of the virus.
MDC research labs: Landthaler, Selbach, N. Rajewsky, Hübner and Gotthardt Labs in collaboration with the Bioinformatics, Genomics, Proteomics, Organoids, Pluripotent Stem Cells and Protein Production & Characterization Platforms
Cooperation partners: Charité – Universitätsmedizin Berlin, Robert Koch Institute, Helmholtz Institute for RNA-based Infection Research (HIRI), the LifeTime consortium with partners in, for example, Italy, Spain and the Netherlands.
What antibodies are formed?
In order to understand the progression of the COVID-19 disease and move vaccine development forward, the lab led by Dr. Kathrin de la Rosa is analyzing how the immune system responds to SARS-CoV-2. Antibodies are an important part of the immune response because they neutralize the virus and thus stop it from entering human cells. What antibodies must be produced for a person to become immune? And what goes wrong when the disease takes a severe course? Can certain antibodies enhance the infection?
“We’re a young lab and wanted to make a difference with our expertise,” de la Rosa says. “Our initial goal is to help develop serological diagnostics.” To this end, the lab is looking to produce relevant viral proteins and specific antibodies and develop testing procedures. Based on this work, the team plans to use blood samples to determine the quality of the antibody response. “We’re searching for what causes particularly severe cases of COVID-19,” de la Rosa explains. “But we’re also learning what properties a vaccine should have to prevent the disease.” For this project, the team is using cell-based and molecular biological high-throughput methods as well as in vitro cultivation of B cells to produce and study antibodies.
MDC research labs: de la Rosa Lab in collaboration with the Protein Production & Characterization Platform
Cooperation partners: Charité – Universitätsmedizin Berlin, Berlin Institute of Health, Kepler University Hospital in Linz
Blocking entry to the cell
The virus enters the body through the nose, mouth or eyes, then latches on cells in the airway that produce a protein called ACE2. Once at this binding site, the SARS-CoV-2 virus infects the cell by fusing its oily membrane with the membrane of the cell and then releasing its genetic material into the cell. Researchers at Freie Universität Berlin (FU Berlin), at the Leibniz-Forschungsinstitut für Molekulare Pharmakologie (FMP) and at the MDC want to find a way to halt this process.
A group led by Professor Rainer Haag at FU Berlin’s Organic Chemistry Division is therefore studying multivalent inhibitors. Professor Christian Hackenberger’s group at the FMP is examining whether substances developed in his lab inhibit interaction between the virus and the cell, which would make them promising targets for antiviral medicines. Professor Michael Bader’s lab at the MDC is already well acquainted with the ACE2 protein and is testing for the same purpose molecules that have been known to bind the protein. It is working with the Dr. Anja Schütz’s Protein Production Platform at the MDC to produce purified ACE2 and to develop additional tools for producing variants of the protein for itself and its cooperation partners.
MDC research labs: Bader Lab in collaboration with the Protein Production & Characterization Platform
Cooperation partners: Freie Universität Berlin, Leibniz-Forschungsinstitut für Molekulare Pharmakologie (FMP)
Disrupting protein interactions
SARS-CoV-2 can only infect people and multiply if various viral proteins repeatedly interact with other viral proteins and human proteins. Researchers are therefore searching for
substances that disrupt these processes. “Due to the emergency situation, we decided to utilize our technology and our know-how to develop a therapeutic molecule,” says Professor Erich Wanker, head of the Proteomics and Molecular Mechanisms of Neurodegenerative Diseases Lab at the MDC.
Anyone who wants to know if two proteins bind together is spoiled for choice with nearly a dozen different methods to choose from. But each method has its own advantages and limitations, and each only measures part of the entire set of protein-protein interactions. Erich Wanker’s lab has developed a technique that merges such subsets into a panorama analysis: “LuTHy” combines two established and complementary assays in one experiment. The combined method detects weak and strong interactions between proteins, as well as direct and indirect ones.
Now the researchers want to use this technique to determine which protein-protein interactions are relevant for the novel coronavirus – and are starting with samples already described for SARS-CoV-1. Next, they plan to search for molecules that effectively disrupt such interactions. This will first entail screening agents that have already been approved by the U.S. Food and Drug Administration (FDA) for other purposes. With the help of the MDC’s computing cluster (MaxCluster), they will also test large libraries of virtual substances – and then conduct lab experiments to determine if the molecules identified can inhibit relevant protein-protein interactions. Tests are being conducted with SARS-CoV-2 at Charité – Universitätsmedizin Berlin to see how promising substances affect the replication of the virus.
MDC research lab: E. Wanker Lab
Cooperation partner: Charité – Universitätsmedizin Berlin
Online tool tracks spread of the pandemic in Germany and around the world
MDC researchers have created an online tool that visualizes the spread of the coronavirus pandemic. Their map displays not only the total number of reported cases, but also the relative number of cases per 100,000 inhabitants for each German state. In addition, people can use a timeline to track the state-by-state development of the pandemic as well as numbers worldwide. The tool, which is freely available at https://covid19germany.mdc-berlin.de, is based on the cases that public health authorities have reported to the Robert Koch Institute (RKI) and the European Centre for Disease Prevention and Control (ECDC).
MDC research lab: Selbach Lab
Further information
- Press release: State-by-state breakdown of COVID-19 in Germany
- MDC in minimal operation – Corona-relevant research continues
- The pan-European LifeTime initiative
Downloadable image
Dr. Emanuel Wyler from the Landthaler Lab uses single-cell sequencing to study how the new SARS virus differs from older strains of the virus. Photo: Felix Petermann, MDC
Contacts
Prof. Markus Landthaler
Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) Berlin Institute for Medical Systems Biology (BIMSB)
Head of the RNA Biology and Posttranscriptional Regulation Lab and Coordinator of Coronavirus Research at the MDC
markus.landthaler@mdc-berlin.de
Jana Schlütter
Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC)
Editor, Communications Department
+49 (0)30 9406 2121
jana.schluetter@mdc-berlin.de or presse@mdc-berlin.de
- The Max Delbrück Center for Molecular Medicine (MDC)
-
The Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) is one of the world’s leading biomedical research institutions. Max Delbrück, a Berlin native, was a Nobel laureate and one of the founders of molecular biology. At the MDC’s locations in Berlin-Buch and Mitte, researchers from some 60 countries analyze the human system – investigating the biological foundations of life from its most elementary building blocks to systems-wide mechanisms. By understanding what regulates or disrupts the dynamic equilibrium in a cell, an organ, or the entire body, we can prevent diseases, diagnose them earlier, and stop their progression with tailored therapies. Patients should benefit as soon as possible from basic research discoveries. The MDC therefore supports spin-off creation and participates in collaborative networks. It works in close partnership with Charité – Universitätsmedizin Berlin in the jointly run Experimental and Clinical Research Center (ECRC), the Berlin Institute of Health (BIH) at Charité, and the German Center for Cardiovascular Research (DZHK). Founded in 1992, the MDC today employs 1,600 people and is funded 90 percent by the German federal government and 10 percent by the State of Berlin.